What is an EDI 835?
Organizations use Electronic Data Interchange (EDI) to communicate electronically with their partner organizations. EDI 835, also known as Health Care Claim Payment/Advice, is an electronic file format used to transmit healthcare claim payment information. This transaction set is used to make payments to healthcare providers and provide Explanations of Benefits (EOB). An EDI 835 document is organized into data elements and segments which include information, such as what charges were paid, mode of payment, and deductible amount.
This electronic data exchange occurs between healthcare organizations, insurance companies, and clearinghouses. The fact that it standardizes the exchange of payment details ensures seamless communication and a significantly reduced need for manual processing.
What components does an EDI 835 file have?
An EDI 835 file consists of several segments, each serving a specific purpose. Here are the key components you’ll find in an X12 EDI 835 file:
- Header Segment: Contains general information about the file, such as sender and receiver identifiers, transaction type, and creation date.
- Provider Level Adjustment: Provides details about any adjustments made at the provider level, such as contractually obligated discounts or refunds.
- Patient Level Adjustment: Specifies adjustments made at the patient level, such as co-pays or deductibles.
- Service Line Information: Contains detailed information about each service rendered, including dates, charges, and payment amounts.
- Claim Level Adjustments: Describes any adjustments made at the claim level, such as penalties or rejections.
- Summary Segment: Summarizes the financial details of the entire payment advice, including total payment amounts and check numbers.
- Footer Segment: Concludes the EDI 835 file, often with control totals and additional administrative information.
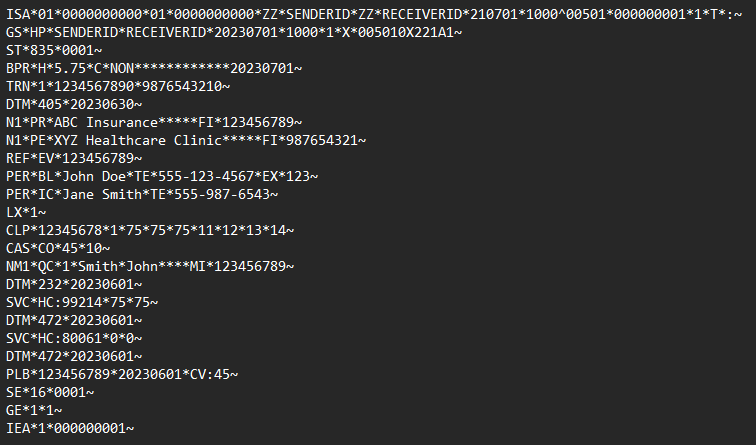
EDI 835 example
To better understand EDI 835, let’s consider an example. Suppose a healthcare provider submits a claim for payment to an insurance company. The insurance company processes the claim and generates an EDI 835 file to communicate the payment details to the healthcare provider. This EDI file would contain information such as the patient’s name, service dates, charges billed, and allowed amounts.
Upon receiving the EDI 835 file, the healthcare provider’s system processes the file, extracting and interpreting the relevant information. This is what an EDI 835 file looks like:
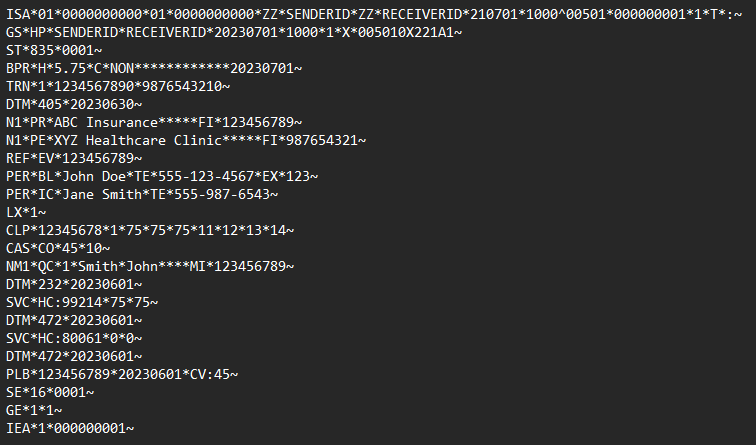
Note: This is only an example EDI 835 file. It does not reflect the exact content or structure of real-world EDI 835 messages.
To acknowledge the receipt of the EDI 835 file, the healthcare provider may send an EDI 997 (Functional Acknowledgment). EDI 997 is a standard acknowledgment EDI that confirms the receipt of the EDI file. However, it does not mean that the trading partner agrees with the contents of the EDI file. So, in this case, it only informs the insurance company that the healthcare provider’s system successfully received the file without any transmission errors.